As you know, patient no-shows are tremendously expensive for healthcare providers, costing $150-$200 per missed appointment and $150 billion annually. To mitigate revenue loss—and save valuable staff time—healthcare managers need to adopt industry tools and best practices.
Tactics like automated reminders and telehealth waitlists can go a long way in recovering lost appointment revenue. According to healthcare IT company Relatient, implementing best practices can help healthcare organizations improve no-show rates by up to 50%.
We consistently see healthcare organizations of varying sizes and structure see upwards of 50% no-show reduction when using best practices and the right systems. [This saves] real money and an enormous amount of time
The Ultimate Guide to Reducing Patient No-Shows” by Relatient
How to define and calculate “no-shows”
A patient “no-show” is an individual who never arrived for a scheduled appointment and gave no notice.
Healthcare managers can calculate the no-show rate—currently at a national average of 8-18%—by dividing total scheduled appointments by total no-shows.
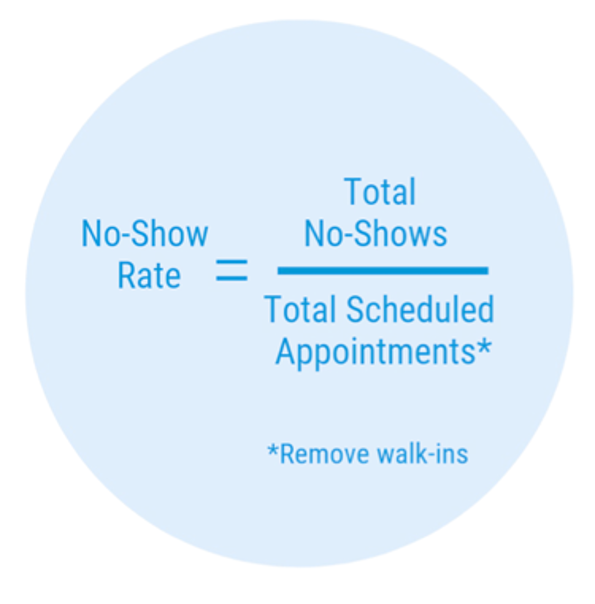
An accurate no-show rate can help managers evaluate lost ROI and benchmark success toward reclaiming revenue. Be sure to avoid the two most common mistakes:
- Including cancellations and appointment changes
- Marking a no-show as “canceled”
Why do patients miss appointments?
Understanding why patients miss appointments can help managers better address pain points. Patients tend to miss appointments for 5 reasons, according to Relatient:
- Forgetfulness
- Inconvenient appointment slots
- Demographic barriers such as age (i.e. an elderly patient who cannot drive) or language
- Anxiety about procedures, bad news, and physician disapproval
- The costs of copays, deductibles, and out-of-pocket expenses
No-showers also tend to fall into one or more of the following categories:
- Single/unmarried
- Under 34 years old or a senior citizen
- Carry no medical coverage
- Suffer a chronic illness
- Located 60+ miles from clinic
How can healthcare managers lower no-show rates and elevate revenue?
10 best practices to reduce patient no-shows
1. Automate appointment reminders
Consider automating your appointment reminders to ensure consistent and strategically timed communication. CRM and marketing automation software such as LeadSquared’s HIPAA Compliant CRM can be very helpful in managing patient availability and message distribution.
Benefits of automated reminders include:
- Reduced risk of communication errors
- Eliminating gaps in communication
- Conserving staff time
- Offering patients a convenient response format
When preparing messages—whether text, email, or phone—consider the following best practices:
- Include provider name and appointment date/time
- Offer easy response options, such as “confirm” or “cancel”
- Prioritize preferred receipt time
- Keep messages brief
- Personalize with patients’ names
This sample SMS text reminder from Practice-Web does a good job of illustrating best practices.
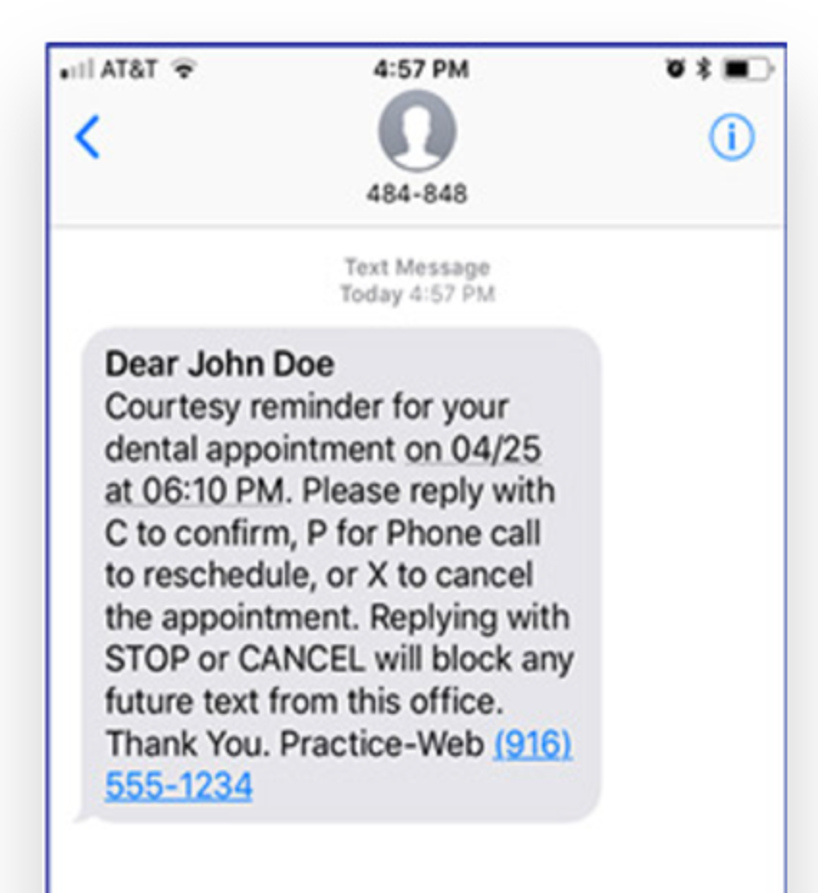
Practice-Web reminds John Doe of his upcoming dental appointment by providing a specific date and time and including several response options (confirm, change, cancel). The text is strategically timed, arriving just as John’s workday concludes.
This email template by Etactics is also a good example of a simple yet effective appointment reminder.
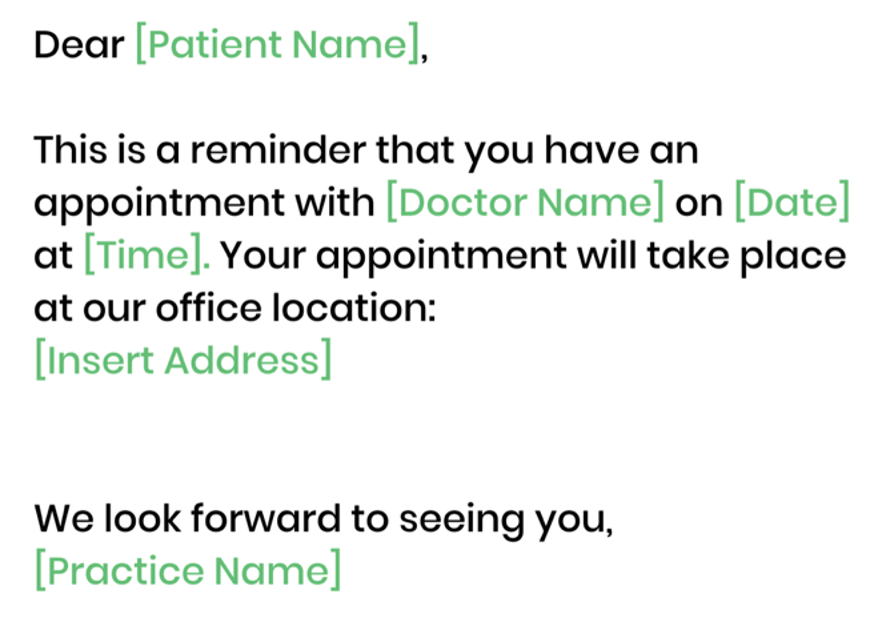
Etactics addresses the patient by name and confirms the specific doctor, date, and time for the appointment. The text also includes the provider’s address for ease of access.
2. Prioritize SMS texting
Consider placing SMS texting at the forefront of your patient engagement strategy. According to a 2017 survey by Becker’s Health IT, more than half of respondents prefer receiving text messages instead of email—and today, 70% of millennials report wanting mobile interaction with providers.
Consider using SMS texting for:
- Appointment reminders
- Follow-up care instructions
- Capturing feedback
- Office notifications and updates
- Bill payment
- Prescription updates
- Ongoing patient education
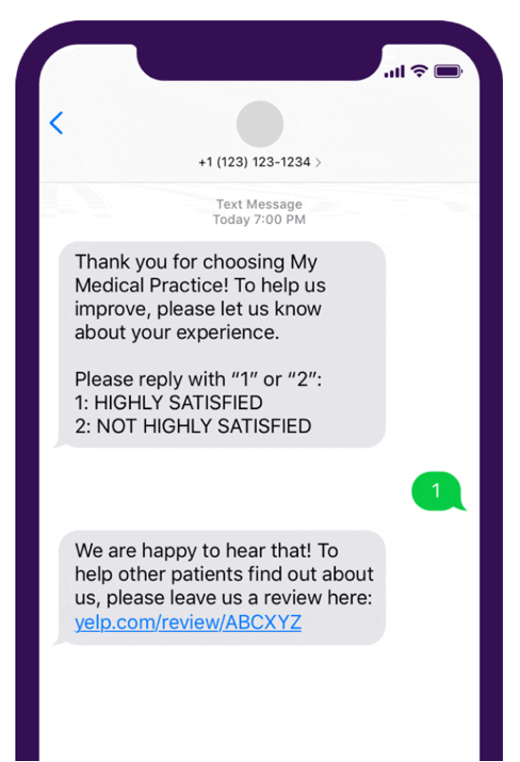
Klara Assistant’s sample text solicits feedback on patient experience. Klara thanks the patient for their business, includes a simple way to offer feedback, and a link to leave a longer review.
3. Use the preferred patient communication method
When a patient schedules an appointment, confirm the preferred communication method. Tailoring communication to patient preference helps ensure messages are received and can improve response rate.
Consider offering message options via:
- Phone (cell and/or home)
- Text
- Mail (i.e. postcard reminders)
When planning your patient engagement strategy, timing is key. Also consider the most effective time to send messages—whether weeks, days, or hours before an appointment.
Aspects to weigh include:
- Lead time before appointment
- Prior communication received
- Desired patient action
4. Employ a compassionate and caring tone
If a patient misses an appointment, approach your follow-up with a caring and friendly tone. Negativity or guilt-tripping can have an adverse effect, potentially causing patients to seek a new provider altogether.
The “sorry we missed you” approach can be especially effective. “Sorry we missed you” is commonly used by sales professionals to inspire customers’ continued business.
For example, check out this sample follow-up email by Etactics.
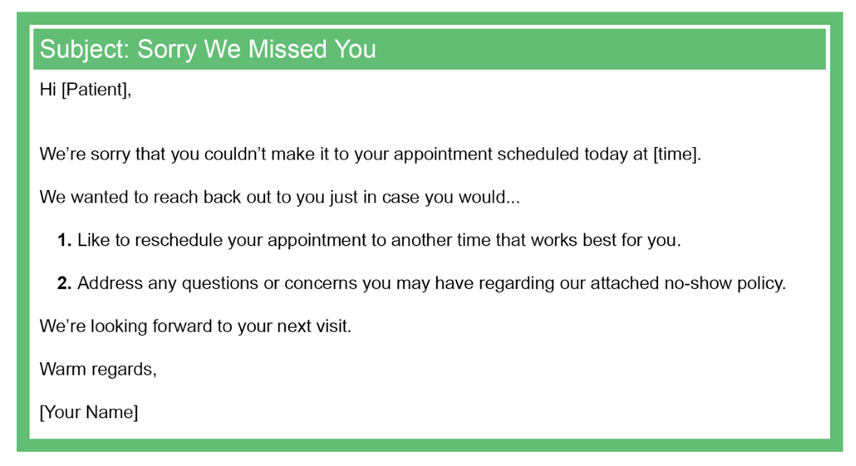
Etactics conveys an empathetic and non-accusatory tone with “we’re sorry” and “looking forward to your next visit,” as well as a “warm regards” conclusion. The sample email also directs patients to the no-show policy and offers a convenient way to reschedule.
5. Implement proactive pay and scheduling
Consider implementing a proactive scheduling policy to help manage patients’ time. Proactive policies require check-ins ahead of appointments, providing a subtle day-of reminder and preventing late arrivals.
Policies might include:
- Arrive 15 minutes before appointment
- Check-in online at least 1 hour before appointment
- Confirm attendance day-of via preferred communication method
You can also help incentivize attendance by allowing patients to pre-pay for appointments. For an additional incentive, consider discounting appointments for patients who pre-pay.
6. Keep wait times short
Short wait times are key to reducing patient no-shows. Vitals’ 9th annual Physician Wait Time Report found 30% of patients abandoned appointments due to long wait times, with 1 in 5 switching doctors entirely.
Appropriate wait times help patients feel respected and valued. To align with the national average, providers should aim for 18 minutes or less.
You might also consider several methods for engaging patients while in the waiting room. Potential ideas include:
- Providing reading material related to visit
- Utilizing tablets for patient reviews
- Offering on-site surveys
7. Provide transportation options
Transportation can be a major deterrent to attending appointments. For required in-person appointments, consider providing public transportation options.
Consider distributing public transit schedules via:
- Pre-appointment materials
- Regular patient communication
- Appointment reminders
- In-office materials, like posters or postcards
Rideshare partnerships can also be a strategic—and lucrative—approach. Hennepin Health’s partnership with Lyft illustrates potential ROI for healthcare providers.
In 2018, Hennepin partnered with Lyft to implement a 12-month pilot rideshare program. The program resulted in a 10% reduction in no-shows—from 31 to 22.5 percent—and a savings of $270,000.
Businesswire
8. Reward those who show up
Positive reinforcement is a powerful motivator. Gestures of appreciation can help strengthen patient relationships, reducing potential no-shows and reinforcing desired behaviors.
To thank loyal patients, consider sending:
- Hand-written thank you notes
- Birthday and holiday cards
- Personalized newsletters
- Anniversary gifts, such as gift cards
You might also consider some more immediate strategies to show appreciation, such as:
- Discounting medical bills
- Hosting monthly giveaways
- Thanking patients on social media or via newsletter
9. Keep a telehealth waitlist
Filling last-minute no-show slots can be tough. As an alternative, consider offering telehealth appointments.
Start by compiling your telehealth waiting list. At each appointment, confirm patients’ typical schedule and create an “on-call” list for no-show slots.
An on-call telehealth list can help:
- Fill empty slots quickly
- Save administrative time
- Avoid no-shows altogether
10. Adopt—and communicate—a no-show policy
A written no-show policy helps set expectations and recover lost revenue from missed appointments. Take care to strategically communicate your policy: In a recent survey, MGMA found 41% of no-show patients were unaware of a no-show policy.
Consider distributing your policy via:
- Website
- Patient communications, such as appointment reminders
- Waiting room
- Hand-outs to no-show patients
Short (1 page or less)—yet specific—policies are typically most effective. Consider including:
- A definition of “no-show”
- Time parameters (i.e. 24-48 hours)
- Specific consequences for missed appointments
- Varied procedures for different patients (established vs. new)
Check out UNC Hospitals Neurology Clinic’s policy for an example.
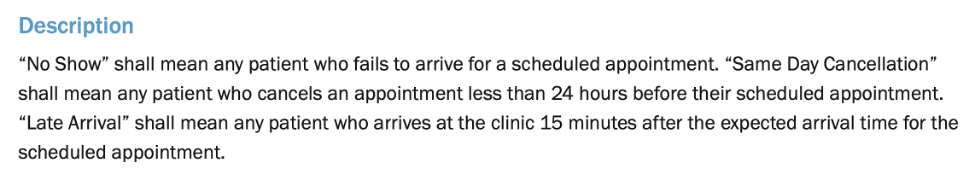
UNC defines “no-show” and provides different levels with “same day cancellation” and “late arrival.” Different no-show levels are assigned different time parameters.
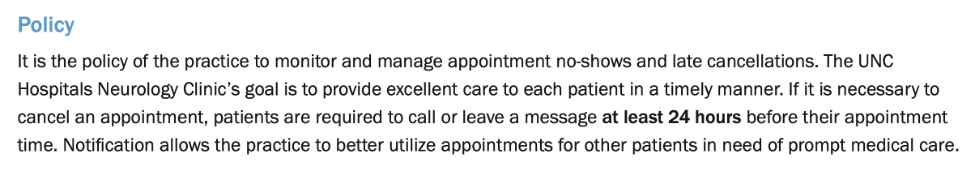
UNC continues by defining a general policy of 24 hours’ notification for cancellations and establishing the clinic’s expectations around patient communication.
Continue building patient relationships
After implementing the above tactics, consider establishing a regular cadence for patient communication and relationship management. Consistent, positive relationships help proactively prevent no-shows—and elevate your brand as a trusted community of care.
Continued tactics might include:
- Soliciting feedback through surveys and online reviews
- Establishing a regular social media presence
- Creating a patient resources newsletter
- Creating online patient communities, like Q&A forums or chat groups









