Medical institutions, like any other business need to have their finances in order to be able to provide continued top-notch care to their patients. Patient Revenue Cycle Management (PRCM), simply put, is the foundation for financial stability for any healthcare institution.
This blog will dive into the details of why effective PRCM is essential, the impact of poor management on a healthcare organization, the current pain points plaguing the process, and how the right CRM can help address all of them.
Patient Revenue Cycle Management in a Nutshell
Patient Revenue Cycle Management is the process of tracking all revenue earned from a patient from the moment an appointment is scheduled to the point the final payment is reconciled. It can be broadly classified into five distinct phases.

Phase 1: Patient registration and pre-authorization
This is the most crucial phase of the Patient Revenue Cycle Management. The key steps involved in this phase are:
Step 1: Patient registration
This is where crucial patient data (such as their name, contact information, and insurance eligibility) is captured.
Step 2: Insurance verification
This is where the patient’s insurance details are verified. The phase also determines the level of coverage the patient’s insurance offers for financial transparency. This ensures a patient is aware of what medical procedures are covered and claims are filed correctly.
Step 3: Pre-authorization
It obtains prior authorization for specific procedures from the insurance.
Phase 2: Documenting and charge capture
This phase focuses on recording and documenting all services and procedures performed to give the patient the care they require. The key steps here are:
Step 1: Identify the services provided.
Step 2: Assign standardized codes (CPT, ICD-10, and HCPCS) for every procedure or service.
Step 3: Document the charges and verify their accuracy.
Step 4: Submit the charges for billing.
Phase 3: Claims submission
This is a critical part of the Patient Revenue Cycle Management, where the healthcare provider now complies and files the necessary claim with the patient’s insurance provider. The key steps involved in this process are:
Step 1: Claim creation
Compile relevant patient and service information.
Step 2: Electronic or paper submission
Send claims to insurers per their specific guidelines.
Once the claims are submitted, it is up to the insurers to adjudicate (review and then decide on whether to disperse or deny) the claims.
Phase 4: Accounts Receivable (AR) management
This phase involves managing payments that have been released by the insurers and adjusting them against the patient’s balance. The key steps involved here are:
Step 1: Payment posting
This is where incoming insurance payouts are recorded and applied to a patient account.
Step 2: AR follow ups
This is where dedicated personnel monitor and follow up on unpaid claims and outstanding payments from insurers and patients, respectively.
Phase 5: Denial management
Denial management is another cornerstone of effective patient revenue lifecycle management. It involves following up on denied claims and investigating the reason behind the denial to mitigate the possibility of further claim denial.
Challenges in Patient Revenue Cycle Management
Healthcare facilities, no matter how well-staffed, trained, and managed do face several challenges with Patient Revenue Cycle Management. The primary paint points here are:
- Incomplete or Inaccurate data capture: Patient pre-registration involves gathering complex data is generally done manually. Any missing information or errors in the captured data lead to a range of issues from delayed or rejected claims to incorrect billing.
- Delayed insurance verification and pre-authorization: Manual verification of insurance coverage and pre-authorization requests impact patient care and the revenue cycle.
- Inaccurate code capture: Assigning inaccurate medical codes can result in the rejection of insurance claims. Inaccurate coding may even result a lower reimbursements, further leading to a loss in revenue (if the claims go through without the error being discovered).
- Inefficient claims submission process: Manual claims filing is time-consuming and can lead to delays in disbursement. Furthermore, navigating different insurers’ submission requirements is complex, and any inconsistencies can lead to claim rejections.
- Lack of transparency: Confusing and complex medical bills can leave patients frustrated and unsure about their financial responsibility which leads to delayed payments.
- Difficulty with patient collections: Following up with patients on unpaid bills is a delicate task but cumbersome when needs to be done manually while walking a fine line between meeting the organization’s bottom line and maintaining positive patient relationships.
The above pain points have a significant impact on both the patient revenue cycle and, more importantly, can cause delays in administering patient care.
How Can a CRM Solution Help?
A CRM specifically designed for the healthcare industry can help address all of the above pain points and significantly improve your patient revenue cycle management process. Here is how:
1. Accurate patient data capture
Specialized healthcare CRMs come integrated with Patient Intake tools that can help capture patient data accurately online. This eliminates the manual data entry process which in turn mitigates the probability of incorrect data entered into the system.
The time saved for your administrative staff can be rather spent on verifying key information to reduce any possibility of problems due to erroneous data down the patient revenue cycle management process.
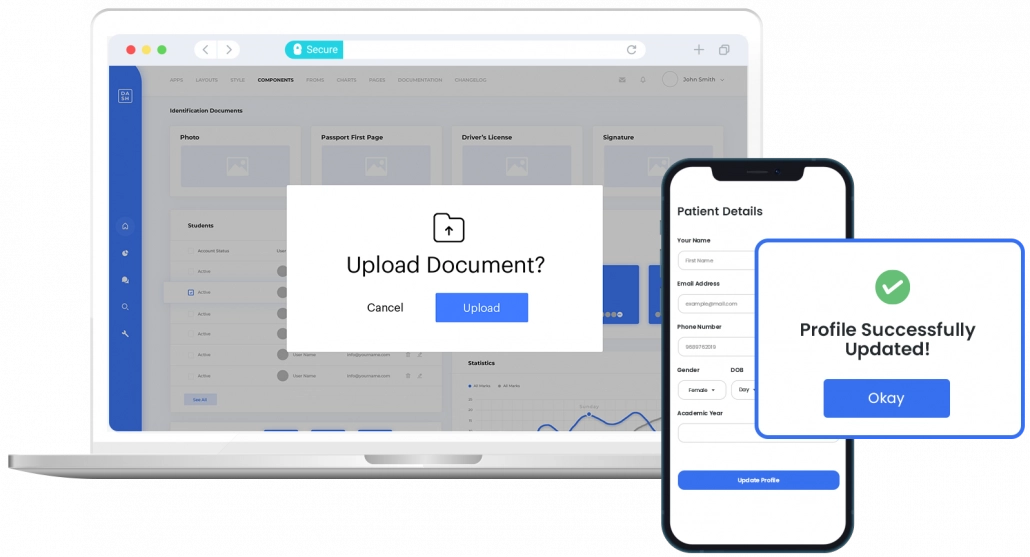
Another significant advantage of dedicated healthcare CRM is that sensitive information is stored in a secure environment. In this regard, LeadSquared’s HIPAA-compliant healthcare CRM is a reliable option. You can manage patient acquisition, intake, and engagement in an all-encompassing platform.
2. Streamlined insurance verification and quicker pre-authorization
Healthcare CRM systems can seamlessly integrate with real-time insurance verification tools. This capability can eliminate any delays that can arise due to a manual process and can also flag any potential coverage issues upfront.
The same real-time verification capability can also speed up the pre-authorization process, enabling timely patient care with complete financial transparency.
3. Decreased claim rejections
Healthcare CRMs are also designed to integrate with Electronic health records (EHR) tools. These tools over and over the ability to automate clinical workflows to improve the overall efficiency of the backend process of patient care and can also assist with accurate code selection for any services rendered.
They ensure minimal inaccuracies when filing claims leading to minimal delays in disbursements and claim denials.
4. Effortless payment collections
CRMs come with a host of automated features that can send out timely reminders to patients without outstanding payments. In addition, they enable the creation of patient-serve patient portals for secure online payments.
This also opens up several payment modes for patients to clear their outstanding bills and improve collection rates for healthcare facilities.
5. Multichannel communication
While this feature may not directly impact patient revenue cycle management, a CRM can provide seamless two-way communication and boost transparency throughout a patient’s entire healthcare journey.
Summing It Up
A dedicated Healthcare CRM can help address several pain points that plague patient revenue cycle management. With one, you can significantly improve your healthcare facilities’ financial health and, as an added bonus, free up valuable time for your medical staff – time that is better spent on providing your patients quality care.
LeadSquared is CRM and marketing automation software built with a vertical-centric, use-case-first approach, which allows it to be easily tailored to the specific needs of various industries. For healthcare institutions, its HIPPA-Compliant CRM system can improve patient relationship management, engagement, and intake for improved Patient revenge cycle management.
Book a Demo to see firsthand what our software can do for you.









