The US telehealth market continues to flourish, with an estimated annual growth rate of nearly 40% over the next five years. Moving forward, Deloitte predicts at least 1 in 4 clinician visits will become virtual.
To offer effective care, healthcare providers must adapt workflows, patient communications, and care expectations. Hybrid healthcare is the “new normal.”
What is hybrid healthcare?
Hybrid healthcare is a medical model which combines in-person and remote care using digital technology, like video conferencing or cell phone apps. Nabta Health, a hybrid healthcare platform for women, offers a more technical definition:
“Hybrid Healthcare [is the] integration of digital health components into traditional care pathways to improve clinical outcomes.”
Sophie Smith, Nabta Health
For providers, “digital health components” might include in-home testing devices, like smart blood glucose meters or body fat monitors. A mail-in Covid-19 test is an especially relevant example.
Why hybrid?
Telehealth services and technology offer patients many potential benefits, including:
- Timely access to care
- Improved convenience
- Cost savings
- Improved provider communication
Take Form Health, a medical weight loss program delivered entirely via a smartphone. Patients are virtually matched with a specialized physician, who conducts a comprehensive medical history review. Patients then receive a personalized plan for weight loss, monitored through their Form Health app.
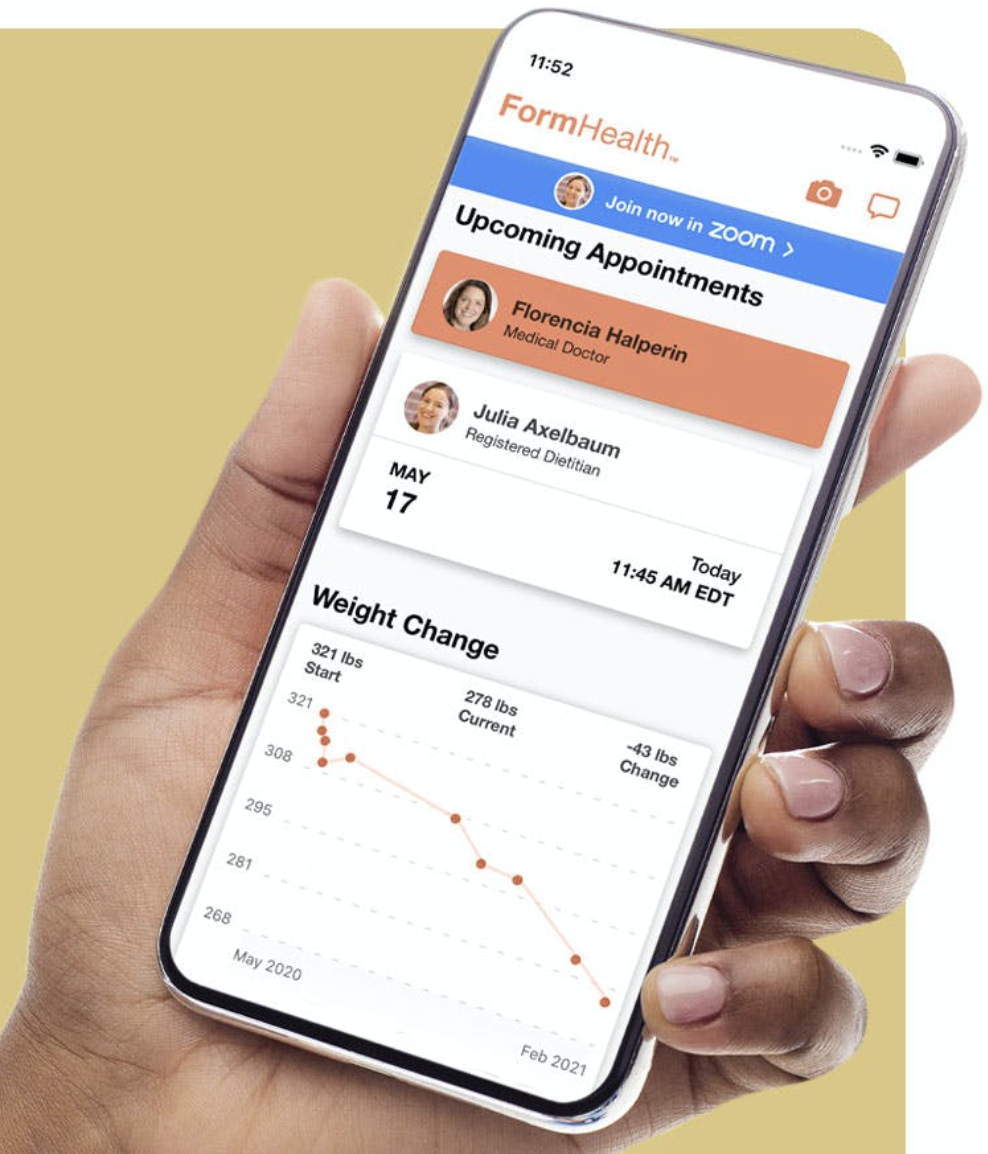
The Form Health app allows patients to track weight loss progress and even monitor upcoming appointments.
Patients receive specialized care without leaving their homes, which saves time and money.
In the report, “The Future of Virtual Health,” Deloitte provides additional virtual health benefits:
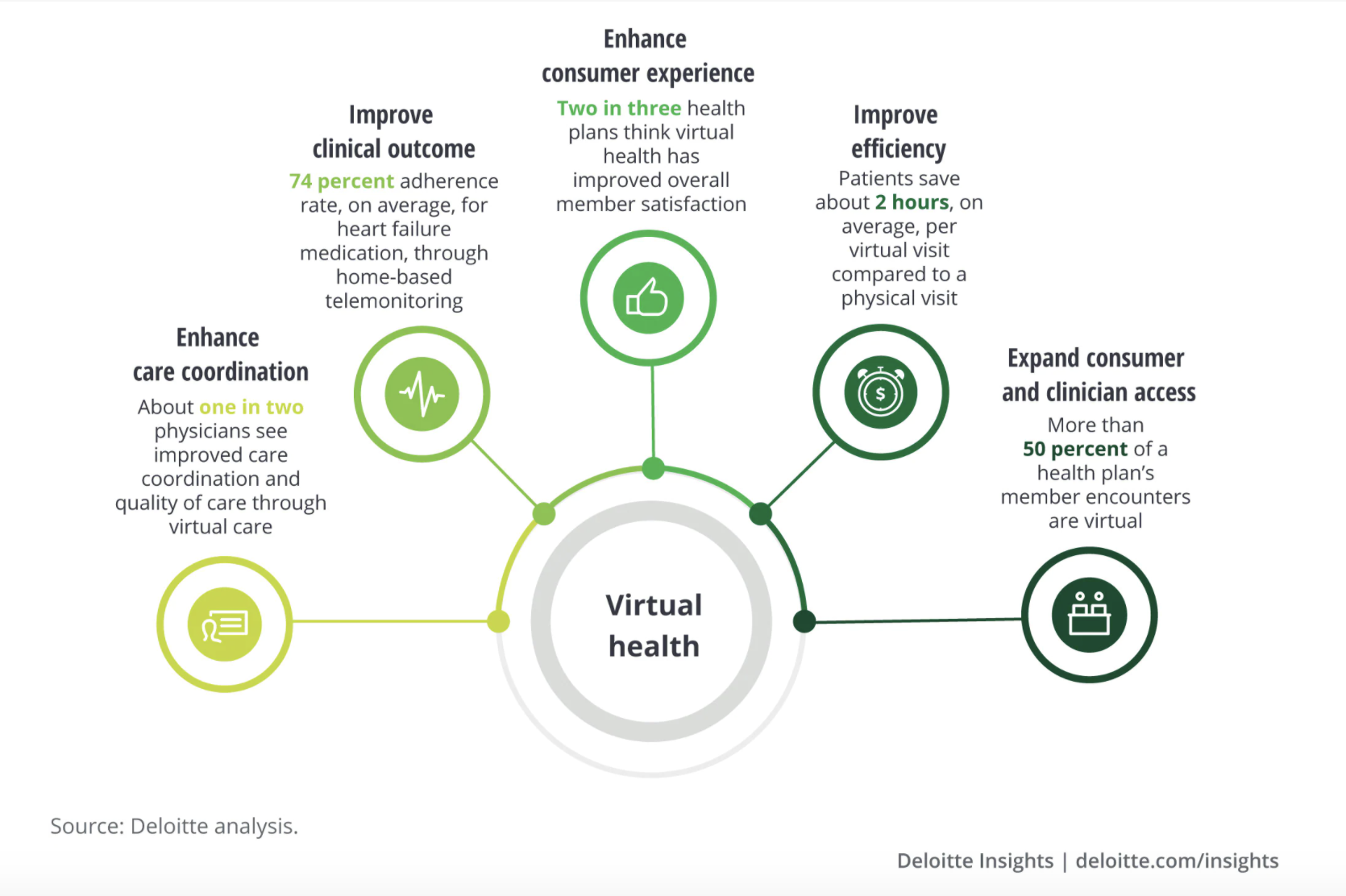
Telehealth will continue to grow
In 2020, investment in virtual health totaled $14.6 billion—nearly double the amount in 2019. On the consumer side, McKinsey & Company estimates up to $250 billion could potentially shift to virtual care.
Healthcare Dive credits telehealth’s continued growth to several key regulatory changes:
- Medicare and Medicaid paying the same rates for virtual and in-person appointments
- HIPAA allowing providers to use “non-public facing communication platforms”
- Commercial players, such as Teledoc or American Well, temporarily removing barriers
The future for telehealth regulations remains unclear, however, with Covid-19 recovery. Providers should track developments which could impact how virtual care is delivered and accessed.
A cultural transformation
The shift to hybrid requires an evolution of the doctor-patient relationship. Traditionally, healthcare providers have owned the care process, determining how and when information is delivered. Telehealth flips the script with patients more in-the-lead.
With remote digital technology, patients can access valuable information—for example, data on infertility, or virus test results—in advance of appointments. Patients can also select appointments and preferred physicians via personalized platforms, creating a new standard of customized care.
How providers can optimize the telehealth experience
1. Prioritize patient education
Patients will likely have questions about telehealth and how the hybrid model may impact their care. Providers should invest in patient education to ensure care options and protocol is clear.
Your website is usually the best place to start. Potential adjustments include:
- Editing messaging to communicate hybrid status
- Publishing blog posts as telehealth resources
- Posting “how-to” instructions for virtual appointments
Take this simple, to-the-point text by the counseling company Two Chairs:
On their homepage, Two Chairs clearly highlights how current care is delivered and what patients can expect moving forward. The text also emphasizes continued convenience and patient choice.
The article, Best Practices for Remote Therapy, is also a good example of patient education. Two Chairs recommends how patients can prepare for remote therapy, with considerations for before, during, and after a session.
Providers should also consider sending updates and resources via social media, email or text. The more touch points with patients, the more opportunities to educate.
2. Invest in an efficient scheduling system
Consumers rank appointment scheduling as a top consideration when recommending a healthcare facility, according to research by Accenture. To attract and retain patients, providers must evolve their scheduling systems.
An effective system prioritizes convenient ways to manage appointments. Patients can:
- Confirm
- Cancel
- Reschedule
- Receive reminder messages
The sample communication below offers a strong example:
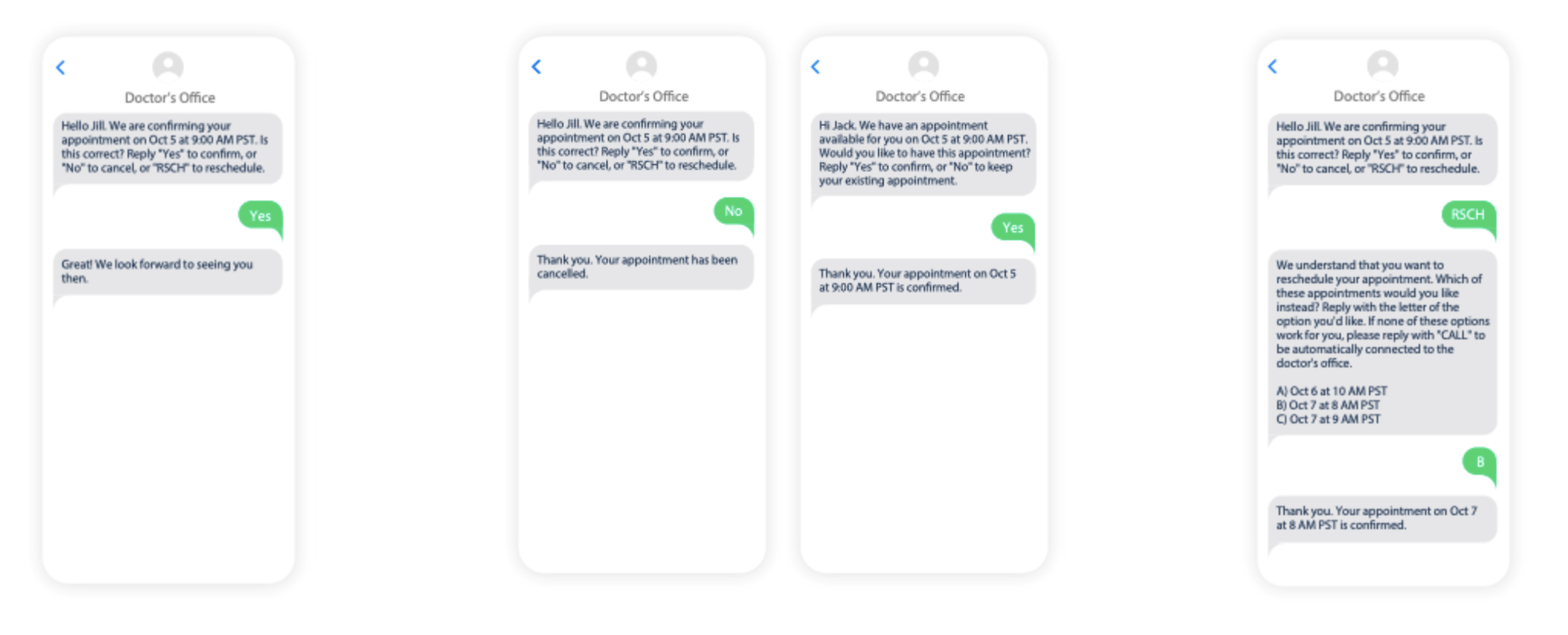
Twilio offers helpful samples in Creating the Future of Hybrid Healthcare.
Patients Jill and Jack can confirm, cancel, and reschedule appointments via text message. Appointments are automatically updated in the scheduling system based on response. Jill is even offered three different options for rescheduling.
3. Offer communication options
You need to investigate how patients prefer to communicate. Using proper channels ensures important information is conveyed effectively.
Research methods might include:
- Asking questions on intake forms
- Conducting online surveys
- Holding a virtual or in-person focus group
Clinicians can use preferred platforms for scheduling (as in the texting example above) and to disseminate key information, such as recommended care services. Providers can also send login links and appointment instructions, and help troubleshoot issues during virtual sessions.
As always, make sure channels are secure and all information exchanged is HIPAA compliant.
4. Ensure services are accessible as possible
By 2030, all baby boomers will be 65+. Yet, only 11% of older adults are comfortable using telehealth technology, according to the American Psychological Association.
Providers can take proactive measures to mitigate confusion or apprehension of telehealth technology. Tips include:
- Initiating mock virtual visits
- Mailing patients printed, step-by-step instructions
- Surveying older adults on concerns and preferences
A simple FAQ page can also help address digital accessibility concerns. Potential FAQs include:
- Is teletherapy effective?
- What are the device and internet requirements?
- How do I access my video session?
- How will my privacy be protected?
5. Refine Your “webside manner”
Body language and facial expressions are typically more difficult to discern on-screen. Physicians should prioritize intentional, empathetic interactions to build trust with patients.
A quiet and distraction-free virtual environment can help. Considerations include:
- Looking directly at the camera to simulate eye contact
- Eliminating background sounds or objects
- Ensuring lighting is glare-free
- Positioning yourself in the center of the frame
Clinicians’ comfort also makes a difference. Providers should maintain proper equipment, posture, and regular stretch breaks—all factors which can impact “webside manner.”
6. Keep cybersecurity top-of-mind
With mobile devices leading telehealth, cybersecurity must remain top-of-mind. Inadequate digital security could result in compromised or stolen patient records.
“When it comes down to it, cybersecurity is a matter of patient safety.”
Dr. Sean Kelly, Chief Medical Officer at Imprivata
Past data breaches exposed patients’ health insurance information and social security numbers, causing significant reputational damage and even lawsuits.
Dr. Kelly, chief medical officer at Imprivata, recommends providers take two key steps:
- Adopt a zero-trust architecture, which entails multiple identity verifications.
- Implement multifactor authentication, which requires verification via different devices.
Hybrid healthcare is here to stay, and providers must adapt to provide effective care. With effective communications and virtual workflows, clinicians can optimize the telehealth experience.
Also read:







